The Challenge of Measuring Pain
Discussed in this article: Medical Cannabis Authorization and Opioid Milligram Equivalents Over Time In Patients with Chronic Pain: A Retrospective Analysis, by Michelle Sexton, ND, et al. Pain Medicine (2025). Open Access.
Pain is one of the great riddles of medicine. It is invisible, subjective, impossible to measure with a ruler or a stopwatch. Do we count the grimaces, the gasps, the sleepless nights?
Because pain is so difficult to pin down, doctors and patients often turn to the medicines themselves for answers. Watching whether opioids or cannabis bring relief, and at what cost.
When it comes to opioids and cannabis, the question is not only which is superior, but whether the two medicines dance together or step on each other’s toes. Do opioids recede when cannabis enters the picture? Or do they march along in tandem, compounding each other’s risks or providing synergistic effects?
Setting the Stage: A Nation in Pain
The scale of opioid use in America is staggering. In 2019, 1 in 5 U.S. adults had a prescription for opioids. Nearly a third of adults report self-medicating with opioids. If those groups are distinct with little overlap, nearly half of adults may be seeking relief with opioids every few months.
And cannabis is not far from this story. Among patients prescribed opioids for pain, cannabis use ranges from 6.2% to 39%, compared with 5.8% in the general population. And studies focused on the cannabis-using population, found that around 65% report using it for pain relief. In other words, people living with pain are turning to cannabis far more often than the average American.
This tangled landscape of how common cannabis use is and co-use with opioids reveals something essential: the choice is rarely either-or. More often, patients may reach for both.
Understanding OME: The Currency of Opioids
“All the opioids have different potencies,” says Dr. Michelle Sexton, lead author of a new UC San Diego study. “We wanted the same unit of measure to be able to measure their use over time.”
That’s where OME — opioid milligram equivalents — comes in. Think of it as the currency exchange rate for opioid medications, taking into account various factors such as route of adminstration. For example, Ten milligrams of oral oxycodone is roughly equal to 15 OME (a 1.5X conversion rate). For a fentanyl transdermal patch, the conversion rate is 100!
By converting every opioid to its morphine equivalent, researchers can track thousands of patients and see whether the OME climbs, falls, or stays stubbornly in place.
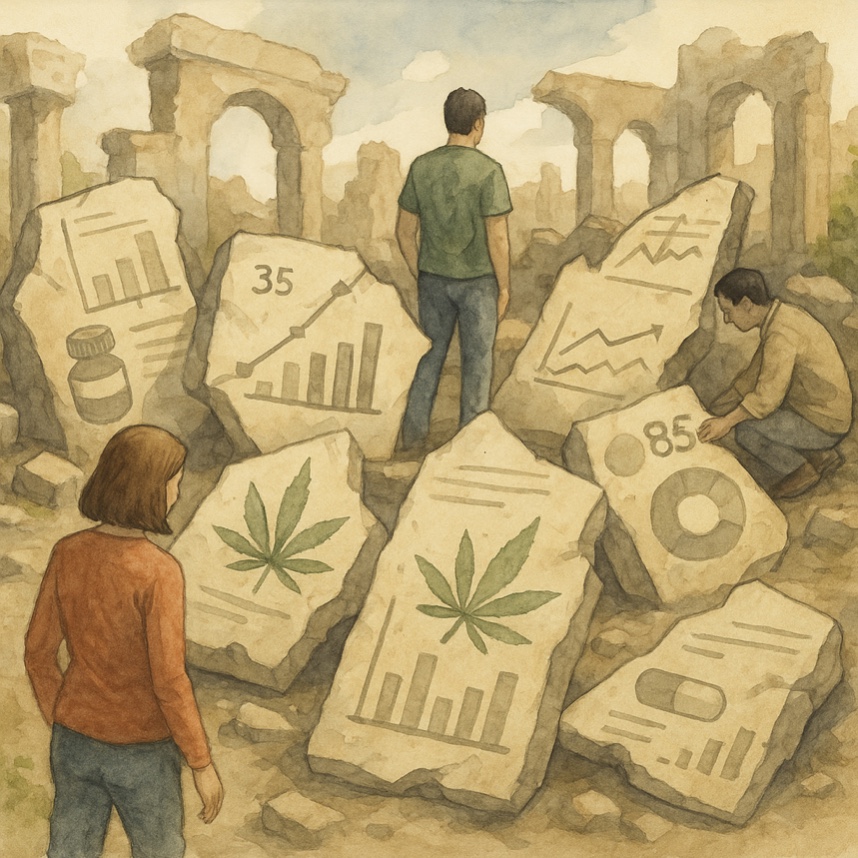
The UCSD Study
Sexton and her colleagues sifted through the records of over 3,000 chronic pain patients from 2016 to 2019. Some had a medical cannabis authorization (MCA); others did not.
Here’s what they found:
- Patients with cannabis authorization averaged about 35 MME/day, compared to 22 MME/day in those without.
- There was no significant increase in OME over time for the entire population
- When stratified for those who received a cannabis authorization, there was no significant reduction in opioid prescribing over time.
- For patients who received a cannabis authorization coupled with a cannabis consultation that included dosing advice, administration and other education (a map through the haze); there was a subtle trend toward lower opioid prescriptions.
Long-term opioid users (LTOU) stayed much higher, at 85 MME/day on average, and their OME was significantly higher if they received a cannabis authorization.
In short: the mere possession of a cannabis authorization from their pain doctor didn’t reduce opioid prescriptions. But pairing cannabis with education and guidance, the door cracked opened for perhaps a different result: less opioid prescribing. This finding is aligned with other research, demonstrating that a conversation with a health professional about cannabis use, leads to better outcomes and less adverse events.
Less Is More
One of the most striking lessons from this research isn’t about whether cannabis works, but how it works. Pain relief with cannabis isn’t a straight line where more equals better — it follows a curve, with benefits peaking at surprisingly modest doses. Meanwhile, many individuals may have an alteration to their psychological response to pain, with improvements in other important outcomes such as sleep quality, functioning and pain relief, things not measured in this study. Integrating patient-reported outcomes that reflect what matters most to individuals using cannabis for chronic pain management is essential for accurately assessing its therapeutic potential and limitations.
“It might seem counterintuitive, but with cannabis for pain, less is often more,” stated Dr. Michelle Sexton. In clinical studies on neuropathic pain, low doses of THC consistently eased symptoms. But when blood levels of THC climbed higher, the benefits in pain control began to slip away.
“Low doses of THC worked well in clinical trials — but as blood levels went up, the pain benefit disappeared.”
This paradox is why Sexton often recommends low-THC products or balanced 1:1 THC:CBD
Formulas or preparations that mirror what has actually been tested in research.
What the Wider Science Shows
If this study leaves you with questions, you’re not alone. The broader scientific record is filled with contradictions:
- Preclinical animal research shows cannabis enhances opioid relief, but human clinical trials have been inconsistent.
- Controlled trials of cannabinoids like nabilone, dronabinol, and nabiximols found no consistent reduction in post-surgical morphine use or cancer-pain opioids.
- Observational studies suggest reductions in prescribing and overdose deaths where cannabis laws exist.
- Some evidence points the other way: opioid and cannabis use rising together, raising concerns about abuse liability.
Myths and Realities
One of the most persistent myths in cannabis culture is that the plant can “cure” opioid addiction. Patients may have reported pain relief, but opioid dependence remained. In Dr. Sexton’s words, “The urban legend is that cannabis cures opioid addiction. Our data didn’t support that hypothesis.”
Another common misconception is that dispensaries should step into the gap left by doctors when it comes to managing opioids. Sexton is clear: this is not the dispensary’s role: “Dispensaries shouldn’t be giving medical advice about opioids,” she notes. “Instead, staff can point patients toward authoritative sources and medical professionals.”
That doesn’t mean dispensaries have no responsibility. On the contrary, she sees a real opportunity for them to help consumers avoid pitfalls — especially around dosing. She has met with patients who were never told how to titrate their products, only to end up with costly, high-dose edibles that offered little benefit or gave significant side effects. “Among other things, it also does economic harm to the patient when they purchase a product that may not have efficacy or causes harm,” she explained.
Looking ahead, Sexton believes the next step is prospective clinical trials to test the opioid-sparing potential of cannabis’ under controlled conditions. She points out that we still don’t know which populations are most likely to benefit. Neuropathic pain may be one candidate.
She also cited research regarding the promise of group medical visits. “People taper off opioids just by being part of a group medical visit,” she notes, adding that cannabis in these settings may work as both a psychological and physiological facilitator to help patients through rebound pain when tapering opioids.
Conclusion
Data sets and their statistics, much like ancient ruins, are fragments of a story. Together they suggest not a miracle cure, but a complicated, shifting relationship between two powerful substances. The data is mixed, the results uneven but the search for safe, effective ways to ease human suffering continues.