“I lay here and I wonder,
what is happening to me now.
After taking my new medicine,
the side-effects are…WOW!!!”
- Michael Howard, Side effects!?!?!
“Roses have thorns, and silver fountains mud; Clouds and eclipses stain both moon and sun, And loathsome canker lives in sweetest bud.”
- William Shakespeare, Sonnet 35
Just as Shakespeare reminds us that beauty can harbor hidden flaws, so too can products like hemp and cannabis carry unexpected risks. For some, what begins as a routine use of a wellness product or medicine spirals into an overwhelming struggle with relentless nausea, stomach pain, and vomiting. This baffling condition is estimated to affect between 350,000 to 2.75 million in the US and is known as Cannabinoid Hyperemesis Syndrome (CHS). This syndrome seems to paradoxically link cannabis and hemp use to these debilitating symptoms.
As cannabinoid use becomes more mainstream, understanding and addressing conditions like CHS is more critical than ever. Thankfully, dedicated researchers, educators, and healthcare professionals are working to unravel this medical enigma. Through their expertise and insights, we can explore the complexities of CHS and the challenges it presents.
The Prevalence is a Growing Concern
CHS cases are increasing, yet many healthcare providers remain unaware of the condition, leading to frequent misdiagnoses and patient frustration. Andrew Peterson, PharmD, PhD, is an accomplished educator and published author in pharmacy management and health policy, and emphasizes the need for healthcare providers to better understand CHS. He points out a crucial gap in clinical practices:
“Since CHS is under or misdiagnosed, the first step is getting healthcare providers to ask patients if they are using cannabis, either medically or recreationally,” said Andrew Peterson, PharmD, PhD, “Data show that even primary care providers trained in medical cannabis don’t always ask about its use, and patients often don’t readily disclose it.”
Imagine bringing your car to a mechanic for a strange noise, only to find they’re unfamiliar with your model. Similarly, doctors unfamiliar with CHS may misdiagnose symptoms, leaving patients feeling lost and confused. To help us grasp the current challenges with CHS, it’s important to examine how our understanding of this syndrome has evolved over the years.
CHS Through the Decades: A Timeline
In 1996, the index case of CHS emerged, though the syndrome remained unidentified until 2004, when it was formally reported in Australia. By 2008, research by Izzo and Camilleri began to illuminate the role of cannabinoids in gastrointestinal and liver diseases, providing a foundation for understanding CHS. In 2013, the first documented case of CHS associated with synthetic cannabinoids was reported, broadening the scope of substances linked to the syndrome.
The legalization of hemp-derived products through the 2018 US Farm Bill spurred the CBD market’s growth while raising concerns about its potential role in CHS. In 2021, CHS symptoms were observed in a patient consuming Δ8-THC gummies, underscoring the potential for CHS with weaker CB1 agonists. By 2022, genomic investigations revealed five significant mutations in CHS patients, affecting cannabinoid metabolism, dopamine regulation, and the TRPV1 receptor, offering critical insights into the syndrome’s pathophysiology.
In 2024, new case reports suggested links between CHS and both CBD use and abrupt cannabis withdrawal. Additionally, the AGA Clinical Practice Update misclassified CHS as a subtype of cyclic vomiting syndrome, highlighting the ongoing challenges of accurate diagnosis and the importance of education in the medical community. While a timeline of CHS may offer us key insights, its root causes remain elusive, as numerous theories attempt to explain its origins.
Theories Behind the Mystery of CHS
While significant strides have been made to identify and track CHS, the exact cause is still a mystery, buried beneath layers of scientific debate. A peculiar symptom is the compulsive urge to take hot showers, thought to provide relief by affecting temperature regulation, perhaps via the TRPV1 receptor channels – cannabinoids are known to stimulate TRPV1 activity. Here are some theories attempting to explain this paradoxical reaction to cannabinoids:
- THC Accumulation: A Delayed Effect?
Some suggest that THC accumulates in fat cells and is slowly released, like a melting glacier. Yet, since CHS usually resolves with abstinence, this theory remains controversial. - CBD: The Wolf in Sheep’s Clothing?
Though CBD is widely hailed for its therapeutic benefits, it might play a role in CHS, as it has been documented with cases. By activating TRPV1 receptors linked to nausea, CBD might be a hidden trigger. However, typical CBD consumption might be too low to cause CHS independently. - Genetic Predisposition: Playing the Hand You’re Dealt
Some individuals may be genetically predisposed to CHS, possessing mutations that affect how their bodies process THC and dopamine. It’s like a card game where some players are dealt a losing hand. - Receptor Rollercoaster: Up, Down, and All Around
Chronic cannabis use might alter cannabinoid receptor sensitivity, like a rollercoaster leaving you dizzy and disoriented, possibly leading to a pro-emetic effect. - An Unknown Additive or Contaminant: What Lurks Beneath
It seems unlikely, but for all we know a factor in CHS could be something unnatural on the plant, such as plant growth regulators or pesticides, or some adulterant or contaminant that is currently evading detection.
- Multiple Classifications: Are There Different Types of CHS?
CHS could very well have several sub-conditions, where certain versions or cases are the result of THC, CBD, genetic or any combination of the above issues. It could be that we will live to see a type 1 CHS or type 2 CHS and so on. Adding to the complexity, some patients report paradoxical symptoms linked to withdrawal from cannabis rather than its use.
Withdrawal or Cessation: An Unexpected Trigger?
There’s an interesting phenomenon where CHS symptoms can be triggered by withdrawal rather than use. “Many patients report that stopping cannabis can trigger symptoms, which paradoxically leads them to resume use to alleviate immediate discomfort,” said Megan Mbengue, RN, a passionate healthcare advocate and founder of Trusted Canna Nurse. She recounts one of her client’s experiences:
“One client, a daily user, developed GI [gastrointestinal] symptoms like nausea and abdominal pain during family vacations when he abstained. Although he never progressed to full CHS, he stopped using after those experiences.”
Despite its complexity, CHS can follow a recognizable pattern in many cases, unfolding in three general stages.
Recognizing the Signs of CHS
Identifying if a patient’s condition follows these three stages could be crucial for tailoring effective treatment. The syndrome typically unfolds in the following three stages:
- Prodrome Phase: Subtle morning nausea and abdominal discomfort. Ironically, patients may increase cannabis use, thinking it will help.
- Hyperemesis Phase: Intense, unrelenting nausea and vomiting take center stage, accompanied by stomach pain and dehydration.
- Recovery Phase: With abstinence, symptoms gradually subside, but relapse can occur if cannabis use resumes.
Pharmacists that regularly provide education on the cannabis caution that the understanding and stages of CHS are not strict categories, and exceptions exist to simplified approaches. Codi Peterson, PharmD, the Chief Science Officer of The Cannigma, shares his insights into the diagnostic complexities of CHS, especially in cases involving withdrawal:
“At this time, it’s unclear if those experiencing hyperemesis during withdrawal are also in a prodromal phase,” noted Codi Peterson, PharmD. “I’ve seen cases where symptoms appear just days after stopping chronic use, making diagnosis even more challenging.”
To further understand current perceptions around CHS diagnostics, we gathered insights from healthcare professionals during a November 2024 Cerium Journal Club Meeting (See pie chart). Participants were polled on key questions about the role of THC screening in diagnosing CHS. The responses highlight the ambiguity and need for more reliable diagnostic methods. Once CHS is identified, patients and clinicians must navigate a variety of treatment options to manage the condition.
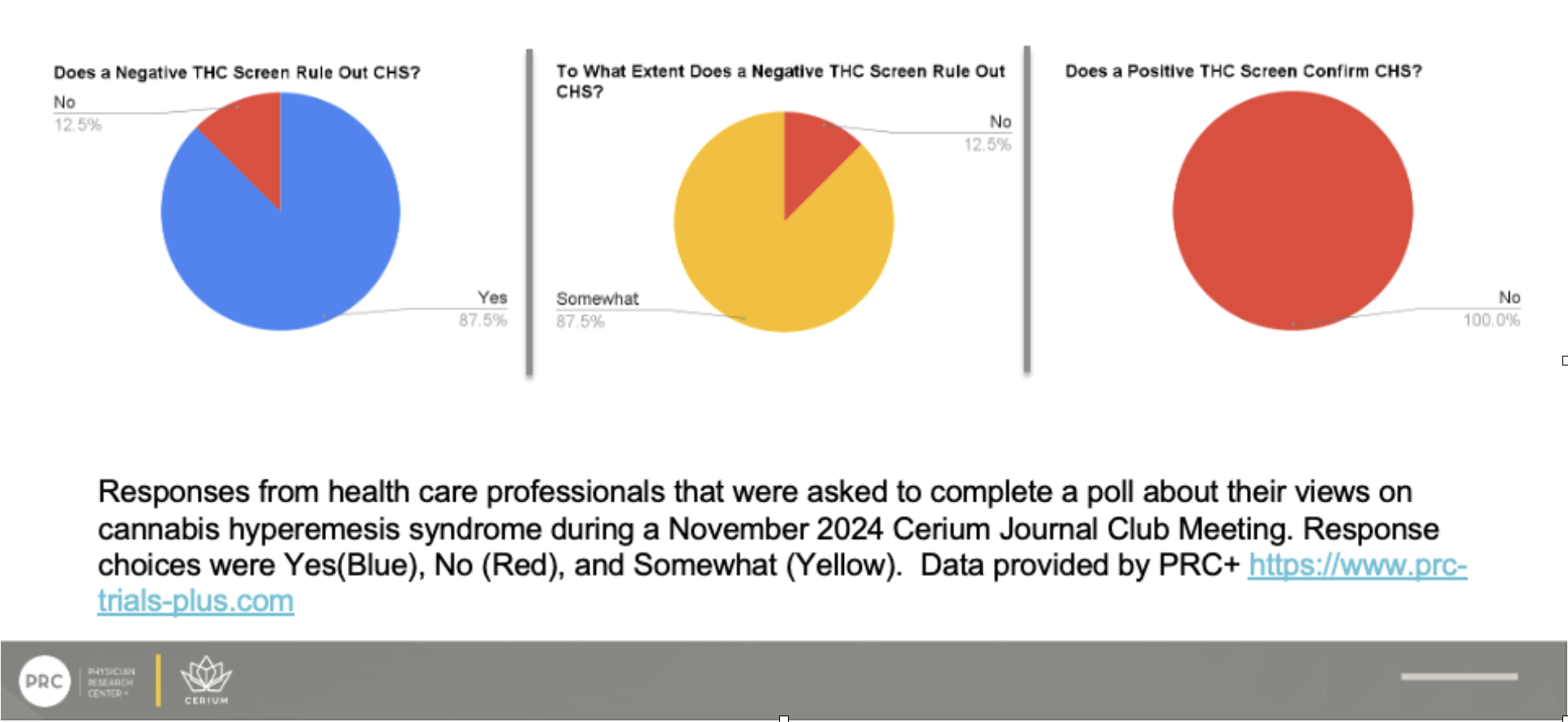
Responses from healthcare professionals about their views on THC screening and CHS. Data provided by PRC+ (https://www.prc-trials-plus.com).
Battling the Beast: A Multi-Pronged Approach
According to clinicians and health professionals, tackling CHS requires a diverse strategy:
- Abstinence: The first and most important step is stopping cannabis or cannabinoid use, like removing a splinter to heal a wound.
- Acute Relief: Medications like intravenous fluids, antiemetics (ondansetron), 5HT3 antagonists, and benzodiazepines (lorazepam) seem ineffective in relieving CHS. Acutely, IV haloperidol and topical capsaicin ointment are reported to have worked best so far.
- Long-Term Defense: Tricyclic antidepressants, such as amitriptyline, are commonly used to reduce relapse risk.
- Psychosocial Support: Cognitive-behavioral therapy aids patients in managing stress, cravings, and developing healthier coping mechanisms.
While battling CHS is difficult, the diagnostic journey itself often poses an even greater obstacle for patients and their doctors.
The Prognosis of Diagnosis
Identifying CHS can be like trying to solve a mystery without all the clues. The condition is often misdiagnosed, with many patients enduring years of unnecessary treatments before discovering the true cause of their symptoms. It is estimated that it can cost over $95,000 in medical bills to finally get a diagnosis, after repeat visits and various tests. This diagnostic challenge is compounded by the fact that many healthcare providers are still unfamiliar with CHS.
Dr. Ethan Russo, a leading expert in cannabinoid science, underscores the importance of addressing misconceptions about cannabis to make meaningful progress:
“Cannabis activists are active counter-productively when making erroneous claims that ‘Cannabis has no side effects.’ Obviously, it does, and these need to be addressed properly in context,” Dr. Russo continues, “THC is a very therapeutic substance but must be utilized judiciously, preferably in low doses to reduce symptoms, and not generate psychoactive sequelae or push tolerance limits. Herbal cannabis contains various other phytocannabinoids and terpenoids that can mitigate risk.”
Russo emphasizes that understanding CHS involves recognizing that cannabis is not suitable for everyone:
“It must also be acknowledged that there are certain people who should not use cannabis, and these include young people at risk for development of schizophrenia and clearly those who are experiencing cannabinoid hyperemesis syndrome symptoms.”
According to Russo, advancing CHS diagnosis and treatment requires a multifaceted research approach:
“It is only with better identification of CHS risk through research on genomic and possibly metabolomic screening and elucidation of its abundant psychiatric co-morbidities and public health implications that progress can be achieved in addressing the problem and devising possible treatment modalities.”
With better diagnostic capabilities and increased awareness, healthcare providers can more efficiently identify and treat CHS, sparing patients years of misdiagnoses and unnecessary treatments. Russo’s work highlights the need for continued research and a balanced perspective on cannabis to develop effective solutions for those affected. Russo’s current focus includes developing a diagnostic test for CHS, which could potentially revolutionize how the condition is identified.
Currently, diagnosing CHS often involves a lengthy process of exclusion, ruling out other gastrointestinal conditions. A reliable diagnostic test would allow clinicians to confirm CHS more quickly, reducing patient suffering. However, advancing this research has not been without its challenges. Due to limited public and industry funding for cannabis-related studies, Russo and his collaborators have had to invest their own resources. Nishi Whiteley, working alongside Dr. Russo, is deeply committed to ensuring the diagnostic test for CHS reaches those who need it most. Reflecting on the team’s priorities, she states:
“We invested over $50,000 of our own money into the CHS study,” explains Nishi Whiteley, who has been working closely with Russo on this project. “He wanted the diagnostic test to be as affordable as possible, so that it could genuinely help patients.”
The team’s commitment is driven by a desire to make the test accessible, not by profit motives. As Whiteley notes:
“There’s nothing wrong with a for-profit corporation doing research. It’s the only way it’s going to get done,” she stated, “So many questions about CHS remain unanswered. We hope over time the anonymized data collected from our commercial kits combined with that from future research projects results in profound insight into the nuances of the syndrome. Such data will ultimately be useful for prevention efforts, quicker diagnosis and better treatment.”
The development of a diagnostic tool could be a game-changer, especially as CHS becomes more prevalent with the increase in cannabis use worldwide. The hope is that with better diagnostic capabilities, healthcare providers can more quickly recognize and treat CHS, sparing patients years of misdiagnoses and unnecessary treatments.
As research continues to shed light on CHS and technology brings us new data sets, awareness and understanding remain crucial for improving outcomes.
A Call for Awareness
CHS is a nuanced condition requiring greater awareness from both the medical community and the public. “There’s still much to learn,” emphasized Megan Mbengue. “The overlap between cannabis withdrawal and CHS, and possible genetic factors, is an area ripe for further research.”
As we move forward, it is essential to bridge gaps in education and research to ensure that CHS sufferers receive the care they need. Together, we can unravel the mystery of CHS and improve outcomes for patients worldwide.
For more Information about CHS, please read this FAQ on Cannabinoid Hyperemesis Syndrome
More about CHS Susceptibility Test: https://what-is-chs.com/
Side effects from cannabis and hemp products can be reported anonymously through www.budsinfo.com
Health Care Professionals Discuss Cannabinoid Hyperemesis Syndrome Case Reports, Prevalence, Assessment, and Interventions:
Disclaimer: This article is intended for informational purposes only and does not constitute medical advice. Always consult a healthcare professional for medical diagnosis or treatment recommendations.